Tackling the big issues around depression
Next to rising levels of depression, society is in the midst of an obesity epidemic. Are they related?
This, and many other big issues, are among the vital research challenges Flinders University researchers are tackling at the Mind and Brain centre at the new flagship South Australian Health and Medical Research Institute in Adelaide.
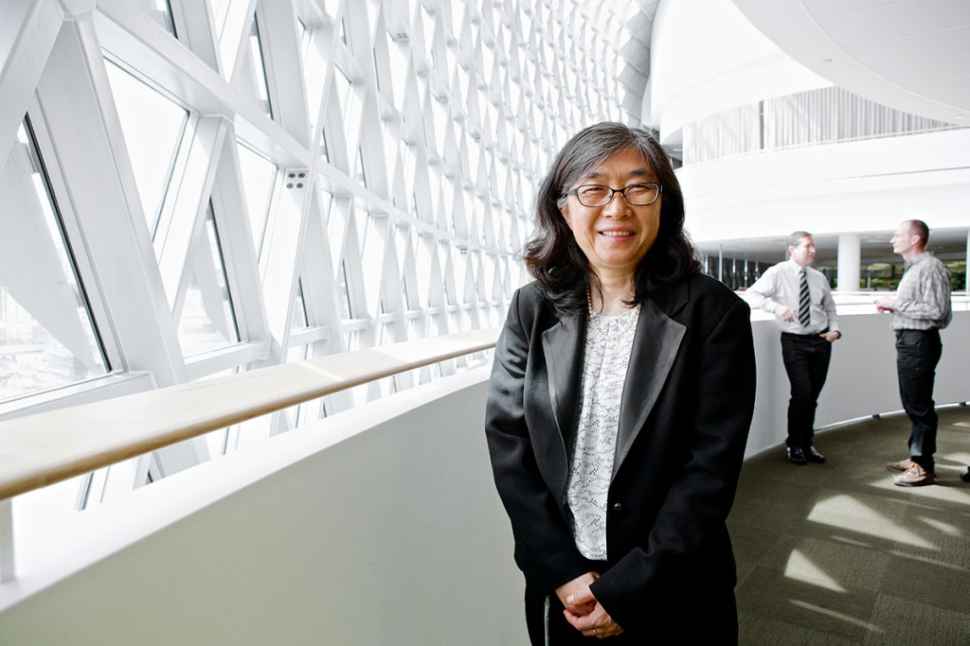
“We are in the midst of both an obesity and depression epidemic,” says Strategic Professor in Psychiatry Ma-Li Wong, who spent more than 20 years researching the biology of depression in Australia and the US.
Correspondingly the rates of people on antidepressants has skyrocketed, says Professor Wong, who notes a rise in antidepressant use in Australia, where more than 20 million prescriptions are made for mental health-related cases a year.
While US health authorities have reported a rise of almost 400% in antidepressant prescribing since 1988, adult obesity rates have doubled from 15% to 30%, underpinning a corresponding explosion in more than 30 serious disease such as heart disease, diabetes and cancer.
But the links between both are largely unexplored and not understood, Professor Wong says. “They are two important topics that don’t operate in isolation and we hope to be able to create the grassroots shift towards holistic management of both.”
Studying the impacts of antidepressants on body weight and body weight regulation with escalating drug use are two aspects of the study.
With major depressive disorder affecting 350 million people worldwide, the stakes are high.
World-leading experts, Professor Wong and Flinders Professor Julio Licinio, believe that obesity and depression must be tackled together in order to develop the breakthrough solutions required to achieve real change in health outcomes.
Their team of exceptional Mind and Brain researchers at SAHMRI are also looking for genetic reasons for depression and stress disorders and individualised treatments for patient care – to name but a few of the major challenges ahead in coming years.
The Mind and Brain team is currently seeking 2,000 participants to assess which antidepressant medication works best for them,
Professor Wong’s pharmacogenomics research project, funded by the NHMRC, is aiming to develop a simple DNA blood test which will lead to more accurate prescriptions for individual treatments.
“With 22 antidepressants covered by the pharmaceutical benefits scheme (PBS), often depression patients have to try several antidepressants before they find the one that works best for them,” Professor Wong says.
“This study is a first of its kind, and will use the genetic variants that appear in the results, to match them with specific types of depression, and if we can better understand the cause of depression we may be able to lessen its future impact.”
The trial involves a 3-4 hour interview to determine the type, frequency, and depth of depression faced by the individual. Healthy people who do not have any serious medical or mental health problems will be used as a control group.
Story by: Tania Bawden